Interviewing and communicating with children

Effective communication with children and young people in clinical settings requires careful consideration of several factors:
Developmental Age: Tailoring the language and complexity of information to match the child’s cognitive and emotional development ensures they can understand and process the information appropriately.
Emotional Temperature: Being sensitive to the emotional context of the conversation helps in delivering messages in a way that minimizes anxiety and supports emotional well-being.
Space and Environment: The physical setting where the communication occurs can impact the child’s comfort and openness. A safe, welcoming, and non-threatening environment is crucial for effective communication.
These considerations help build trust and facilitate a more productive and supportive interaction between clinicians and young patients. Children are not miniature adults; their understanding and interpretation of speech can vary significantly, especially when they are younger than 10 years old.
We conducted a research study titled “Information sharing experiences of professionals looking after children with cancer: A qualitative exploration from a Specialist pediatric oncology unit in India”.
The themes that emerged from the above study are as follows:
- Information Needs of Children vs Adolescents are different:
- Children were primarily concerned about immediate issues (“here and now”) related to their condition.
- Adolescents, on the other hand, expressed worries about the broader impact of cancer on their lives, including friendships and academics.
- Parents’ Information Needs may vary:
- Parents, particularly mothers and fathers, had different information needs.
- Mothers and fathers were curious about treatment outcomes, costs, and effectiveness, reflecting distinct patterns in their information-seeking behaviors.
- The nature of information expected by children and their caregivers changes over time:
- Information needs varied significantly across different stages of treatment (start, during, remission, end-of-life).
- This dynamic nature required healthcare professionals to adapt their communication strategies accordingly.
- Impact of the clinicians’ journey as a professional influences communication:
- The personal experiences and journeys of clinicians themselves influenced their approaches to sharing information with families and patients.
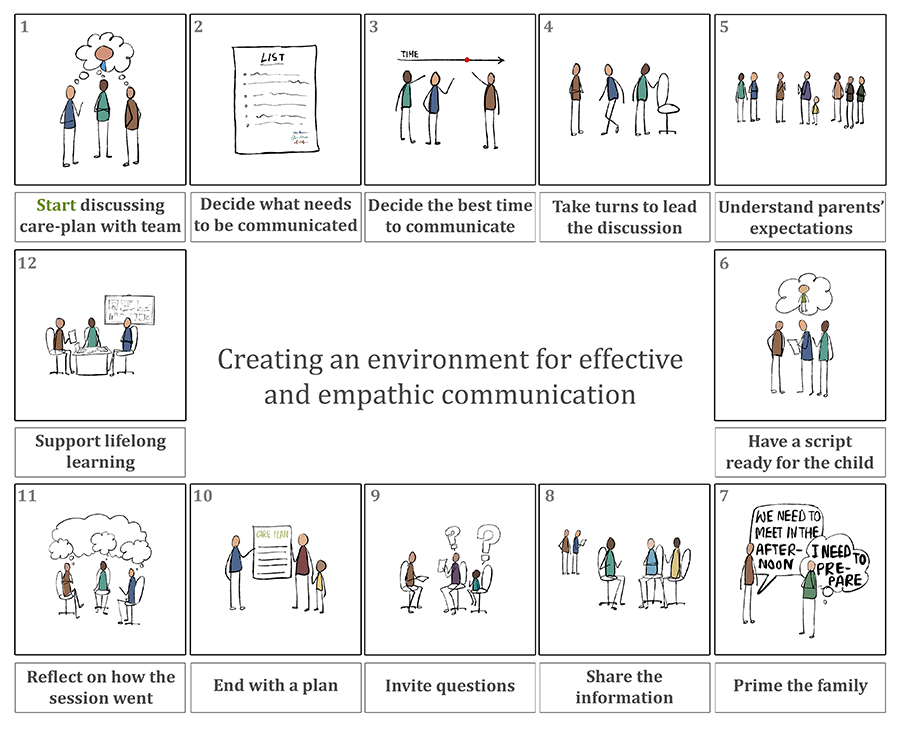
- Direct observations of Consultations led to greater insights into communication preferences:
- Direct observations highlighted effective practices in information sharing:
- Priming parents before delivering critical information may help when delivering bad news.
- Involving multiple family members during discussions when done with sensitivity may create a cordon of care around the child and his immediate family.
- Clinicians should try to manage intense emotions expressed during these discussions.
These themes underscore the complex and evolving nature of information sharing in pediatric oncology settings, emphasizing the importance of tailored communication strategies that consider the developmental stages of patients, the specific concerns of parents, and the emotional dynamics of consultations.
A culture of open communication in a paediatric oncology team provides a stable foundation of care for children and their families and creates a harmonious work environment.
References
Datta, S.S. (2023) Children with cancer: Are we healing the body & missing the mind? Indian J of Medical Research 158(4): 327-329 DOI: 10.4103/ijmr.ijmr_1870_23 (Access here)
Chaudhuri T, Nandakumar D, Datta SS, Husain Z, Sukumaran R, Yadav IS, Krishnan S, Panda S (2022) Information-sharing experiences of professionals looking after children with cancer: a qualitative exploration from a specialist paediatric oncology unit in India ecancer 16 1399. DOI: 10.3332/ecancer.2022.1399
